"Hitachi's answer was so appealing. I knew right away this would make a doctor's job much easier" says Chikashi Ishioka, Vice-Director of the Tohoku University Hospital.
Tohoku University Hospital (TUH) is one of the university hospitals in Japan that is putting much effort into cutting-edge cancer treatment. Starting with world-leading genome cohort research, the university is taking on one challenge after another in new areas of research covered by Future Medicine, epitomized by the school's outstanding achievements in genomic medicine, basic life sciences, and information science research. However, undertaking these efforts while operating day-to-day medical service is a challenge itself amid outcries about the shortage of medical doctors. This is where the latest technologies come in, to reduce the busy medical doctors’ workload. This could make it possible to pursue initiatives for making further progress in healthcare, including considerations of advanced treatment options.
Aiming to fulfill its mission to accelerate the widespread use of cutting-edge healthcare, TUH and Hitachi have engaged in various collaborative creation projects. This includes installing a supercomputer that serves in personalized and preventative healthcare. This case study introduces an initiative that reduces the workload of medical professionals by supporting efficiency improvements to cancer genome medicine. It has the potential for providing more patients with the option of cancer genome medicine, which currently can only be applied to limited patients.

Photograph provided by Tohoku University Hospital
Before going into the details, here is a brief explanation of the current situation in cancer treatment. Cancer is the most common cause of death in Japan, with one out of two people contracting cancer in their lives. Healthcare workers are constantly exerting every effort to save the lives of many cancer patients.
Cancer strikes many organs of the body. In traditional treatment, the type of therapies and drugs are selected according to the primary cancer organ, such as breast cancer and lung cancer. Recent research, however, has shown that even for cancers from the same organ, genetic variations can result in varying drug effects and side effects. For this reason, the emergence of highly precise personalized medicine tailored to each unique patient characteristics such as the patient's genetic variations is expected to play an important role in deciding on different treatments, even for cancers of the same organ.
As personalized medicine goes forward, cancer gene panel testing, which investigate hundreds of genetic variations related to cancer in a single test, have recently come into use. Because these tests make it possible to select optimal treatment options in accordance with the type of genetic variations, they may be the gateway to cancer genome medicine and are garnering attention as the key to the widespread use of personalized medicine. In June 2019, Japan's national health insurance began reimbursement for patients meeting certain criteria of these testing.
Cancer gene panel testing ran into a big issue in its implementation. As Dr. Ishioka says: "The load put on healthcare workers is enormous."
After a cancer gene panel testing is conducted, a meeting called a "Molecular Tumor Board" views the test results and decides on optimal drugs and treatment options. In addition to the attending physician, many others participate in the meeting, including medical oncologists, specialists in genetic medicine and pathology, and medical practitioners trained in genetic counseling. After verifying the test results from these various perspectives, this group then decides on a treatment options that could be appropriate for the individual patient.
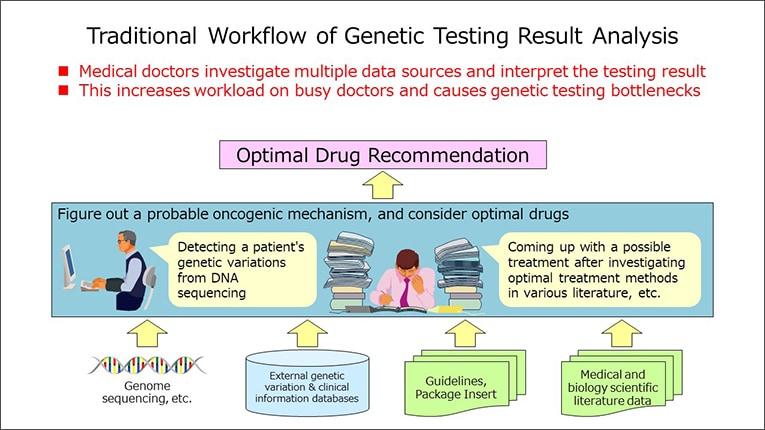
The part of this procedure that put a particularly large load on healthcare workers is the creation of the report used in the MTB discussions. Analyzing the results of cancer gene panel testing reveals necessary information on genetic variations that is based on patient cancer tissue. However, MTB discussions require other information as well. Based on the patient's treatment history and health status, it is also crucial to investigate recent research papers, searching for and analyzing information on the results of the latest treatments outside of standard treatments, clinical trials, and other pertinent materials, and then to compile all this with the test information into one report.
Moreover, with various specialists participating in expert test panel discussions, the fact that each specialty has its own technical terms itself becomes an issue. Unifying terminology therefore also requires consideration.
According to Dr. Ishioka, creating a report required medical doctors to spend several days including spare moments in their regular practice. It is no wonder that participating physicians are subject to a tiring workload.

Chikashi Ishioka, Vice-director of Tohoku University Hospital
Photograph: Akihiro Murakami
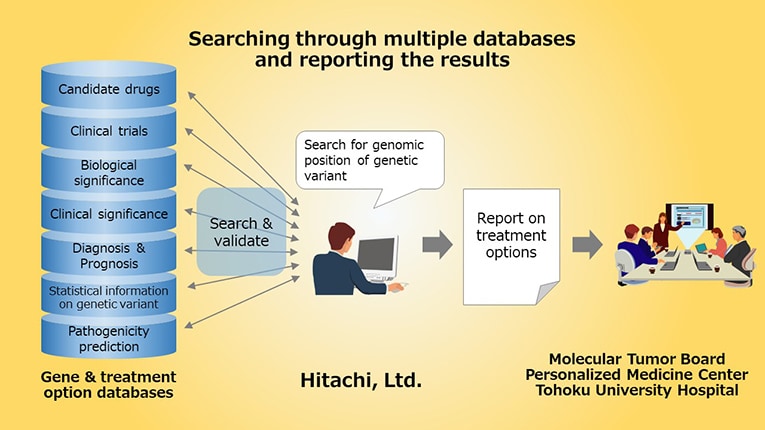
To solve these issues, Hitachi proposed and developed its Molecular Tumor Board Support System. Reports created by this system have succeeded dramatically in making it easier for medical professionals to understand. According to Dr. Ishioka, the reports "not only had a well-organized layout that allows required information to be quickly found, but even supplemental information was also easily searchable. I feel this to be the fruition of Hitachi's propriety expertise."
He goes on to say: "It is important for medical staffs who see the report to be able to immediately identify all the important information. It is sufficient for them to look over parts that provide useful information as necessary." The system takes into consideration the need for healthcare workers to quickly gain understanding from a copious amount of information.
Worthy of mention is that the reports are not only easy to view, but they can also be created nearly automatically. Healthcare workers, released from the work of creating a new report for each patient, need to only go over reports created by means of the support system. Reports that healthcare workers used to create over the several days can now be created in just a few hours by searching a genome test report database.
What factors drove the success of this creative collaboration with Tohoku University?
The biggest contributor was the commitment and enthusiasm of Hitachi’s engineers to build a good system based on thorough knowledge of the practical work being done. In addition to listening to the voice of those who work in the frontlines, they also conducted detailed interviews on the situation of the MTB and scrutinized all necessary information piece by piece. According to Eiji Kanamori of the Hitachi Healthcare Solution Division, "Our longtime relationship allowed us to communicate smoothly between industry and academia. I think this is how we were able to build a good system." Hitachi’s stance of valuing knowledge from the field is reflected in its recent focus in the in-house development of variant scientists (human genome analysis specialists).
Another key to success was the high technological capability and the extensive expertise that Hitachi possesses in the building and operation of large-scale supercomputers. Tohoku University's Tohoku Medical Megabank Organization (ToMMo), established in 2012, created a biobank of about 15,000 people and carries out research involving service for personalized and preventative healthcare. The platform for this, the Supercomputer for Genome Medical Science, was built by Hitachi and continues to run smoothly. Hitachi has the expertise operating hundreds of calculation servers in order to continuously process up to several tens of millions of data analysis requests, and this know-how has also been passed on to the building of the support system.
The Molecular Tumor Board Support System was developed based on thorough knowledge of the practical work that’s occurring on the frontlines.

Even after completion of the Molecular Tumor Board Support System, TUH wants to continue partnering with Hitachi to develop systems that contribute to patient needs and enhanced quality of life (QoL). Personalized medicine is more than just cancer genome medicine. According to Dr. Ishioka: "Taking the cancer genome as a foothold, we would like for Hitachi to develop tools that perform integrated analysis of the comprehensive analysis of various types of biological materials."
Personal values and lifestyles are also major factors in formulating treatment policies and personalized medicine. "Take drug A, which, for example, is effective against a certain disease. If it is accompanied by pain, the patient may prefer not to use it. Or if it's expensive, it might not be actively used because of a patient policy of wanting to lower overall medical costs. In regular medical practice, obtaining patient’s understanding while taking these various parameters into account is difficult. If we can incorporate this kind of information into a healthcare support system in the future, we should be able to create patient-oriented personalized medicine to an even higher degree." In response to the needs of healthcare workers, Hitachi will continue to accelerate new avenues for genome medicine in Japan.

Photograph: Akihiro Murakami
Release Date: March 2020
Solutions By: Healthcare Business Unit, Hitachi, Ltd.







